“That’s just my OCD!” I’ve heard that phrase many times amongst my peers whenever they would describe a particular habit. I was aware of the fact that none of us had actually seen what OCD is actually like. However, over the last few weeks, our family has witnessed some significant signs of OCD in Anjali’s behavior. This led me to learn more about what the condition is, so let’s dive right into what I discovered!
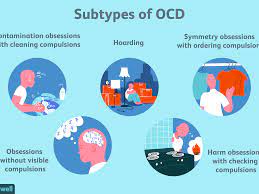
Obsessive-Compulsive Disorder encompasses a large variety of specific phobias or compulsive and sensory requirements. This can morph into unique requirements for a given individual, including specific ordering of items in their daily lives, visual requirements, repetition of some simple activity, and much more. A Mayo Clinic article explains that the main symptoms for OCD include “Fear of being contaminated by touching objects others have touched . . . Doubts that you’ve locked the door or turned off the stove . . . Intense stress when objects aren’t orderly or facing a certain way,” and a variety of other examples. Additionally, the International OCD Foundation reports that “About half a million children in the United States suffer from OCD. This means that about one in 200 children, or four to five children in an average-sized elementary school.”
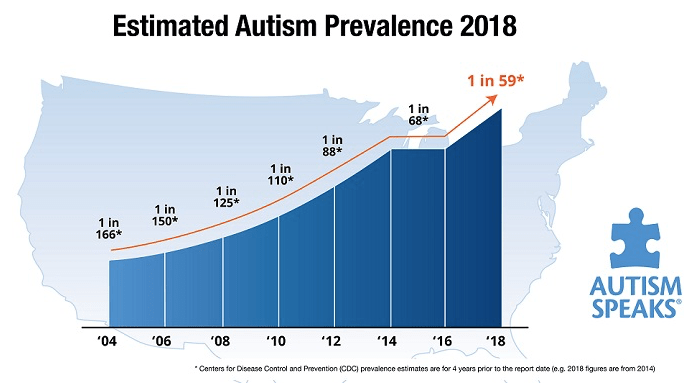
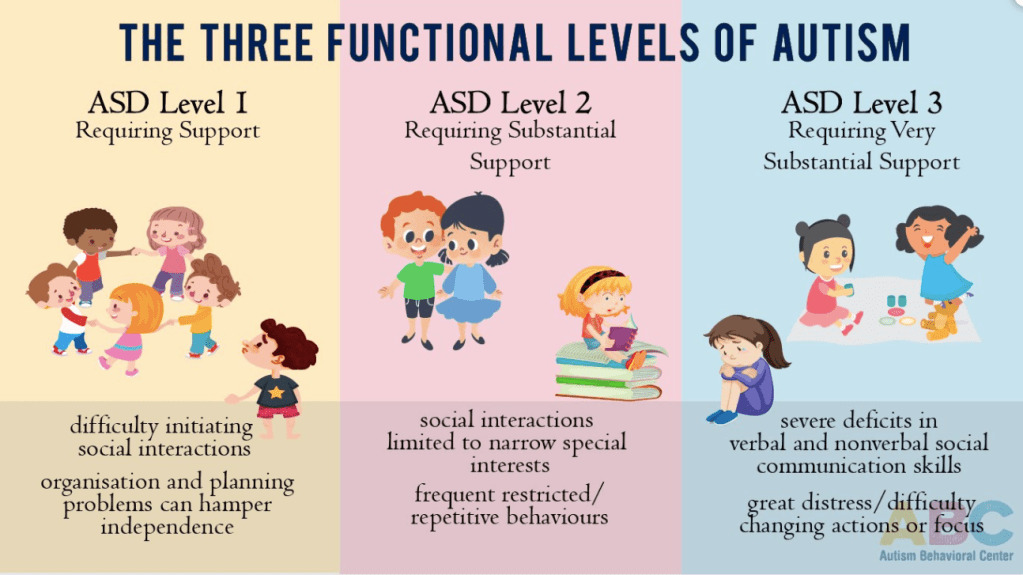
So how does OCD link with ASD? The prevalence of both of these diagnoses has significant overlap. A study published in PLOS ONE, a well-reputed peer-review journal, suggests that “people with autism are twice as likely to receive a diagnosis of OCD and people with OCD are four times as likely to also have autism.” So what does all of this mean for Anjali? First and foremost, I want to emphasize that she has not yet been diagnosed with OCD, and in no way am I implying that she is a definite case of OCD. It’s important for everyone to understand that a pediatrician is the only individual who can assign this diagnosis to an individual.
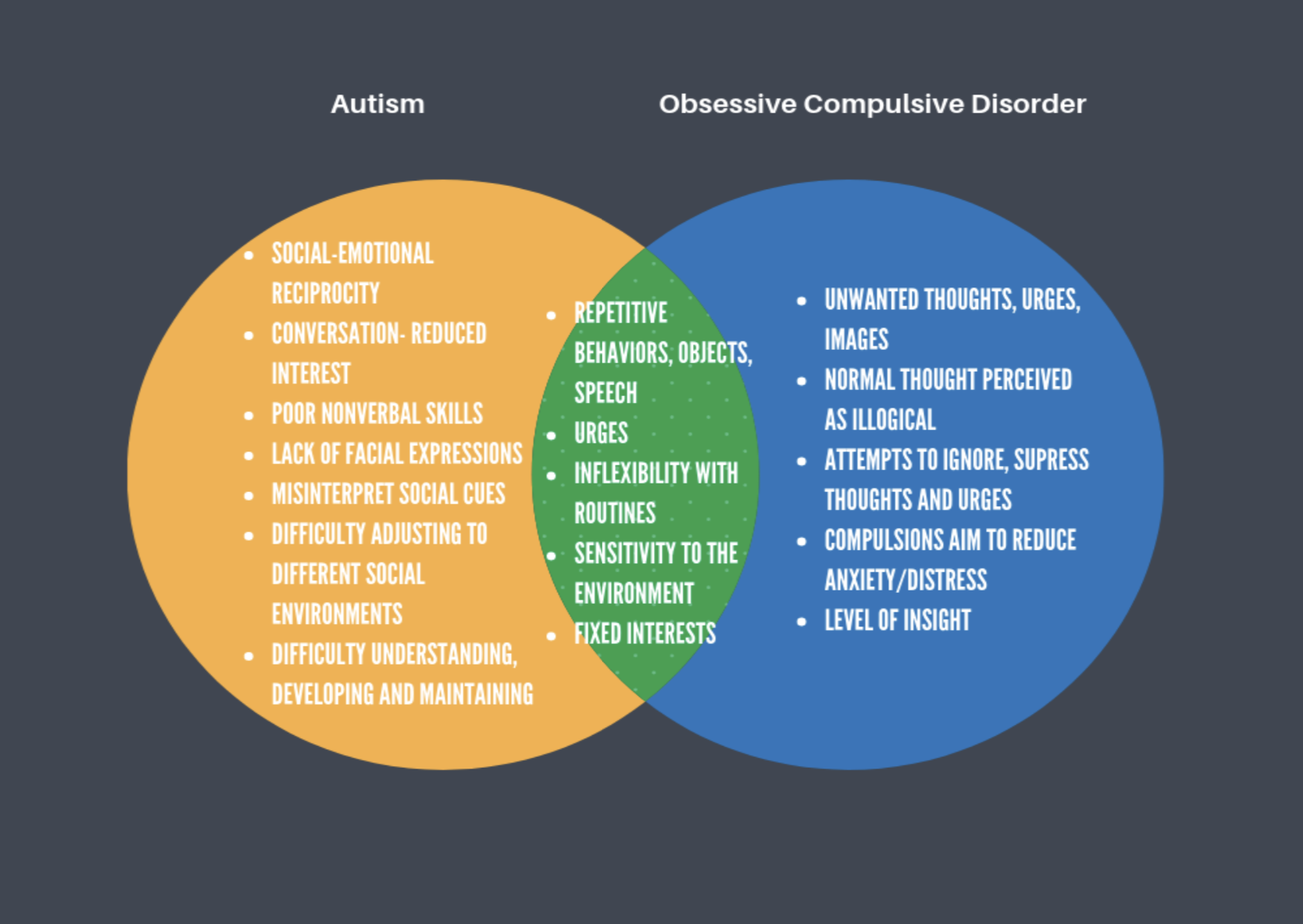
However, Anjali has shown some signs that have led us to seek a professional’s evaluation of her behavior. Her repetitive and compulsive actions include opening and closing of bedroom doors, wanting doors locked (or unlocked, depending on the day), wanting specific water temperatures, and wanting certain rooms to always be dark. It’s been quite challenging and frustrating for everyone in our family to adjust. She seems to be developing new phobias and requirements every day, while also maintaining previous behavioral patterns. Do we have it figured out? Absolutely not. However, that’s the message I want to highlight to all of you. If a special needs family member is showing OCD symptoms, it’s important to seek a physician’s evaluation of the case, while also remaining calm and patient during this period of adjustment!

:max_bytes(150000):strip_icc()/autism-during-the-covid-19-pandemic-4842556-color01-e5ba5b3674d0409797d3a04475b9bbfe.gif)